Introduction
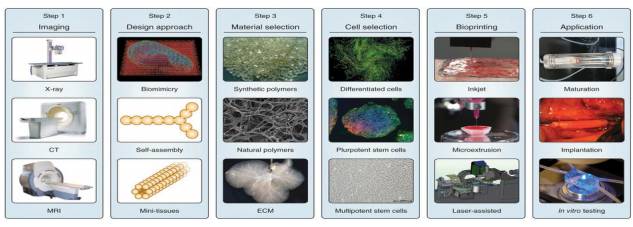
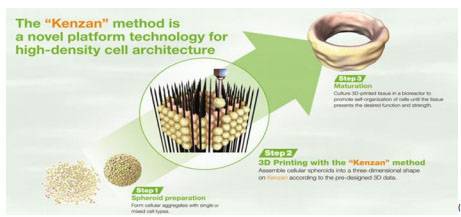
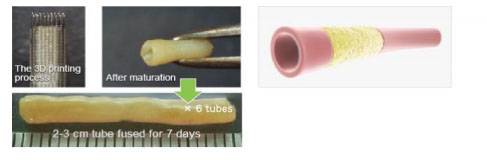
The WHO defines health as “A state of complete physical, mental and social wellbeing, and not merely the absence of any disease or infirmity.” The failure of physical health is, at most times, one of the major causes of death or debilitation. The idea of replaceable, artificially engineered, biocompatible body parts and organs, which might have been a pipe dream for every science fiction lover, has gradually emerged as one of the front-runners in research over the last half a decade. In a world where there is a gross variation in the kind of lifestyle from person to person, there is a need for customizable parts that are both compatible and also suit the specific requirements of the individual. Three-dimensional printing provides precise control, and can be used with a large number of biological structures. Various organs can be printed and sustained in a lab grown environment, of which the tissue level in two dimensions is the easiest to achieve and can be used in drug interaction testing. However, the end game in the field is the successful bioprinting of three-dimensional organ level structures with adequate vasculature, as cells that are more than around 200 micrometers — a couple of human-hair widths — away from a source of nutrients quickly die. Therefore, creating a realistic vascular system will be necessary if researchers are to successfully build organs. Such a system can sustain the organs independent of a lab, and can be used for organ transplants; which, as futuristic as it sounds, could one day result in quasi-immortality; as all failing organs could be replaced as and when required to further prolong one’s life as long as one wishes to.